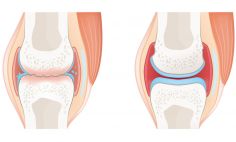
Rheumatoid Arthritis (RA) is a tricky disease. No one knows what causes it, but while there isn't yet a cure for the autoimmune disease, it can be treated. Arthritis is an extremely common problem but not all forms of arthritis are alike.
Just as symptoms of RA can vary, medical treatments can vary, but the important thing to know is that over the last 20 years the treatment of RA has changed dramatically with the approval of many new, highly effective drugs.
"We now have better treatment therapies to keep you safe."
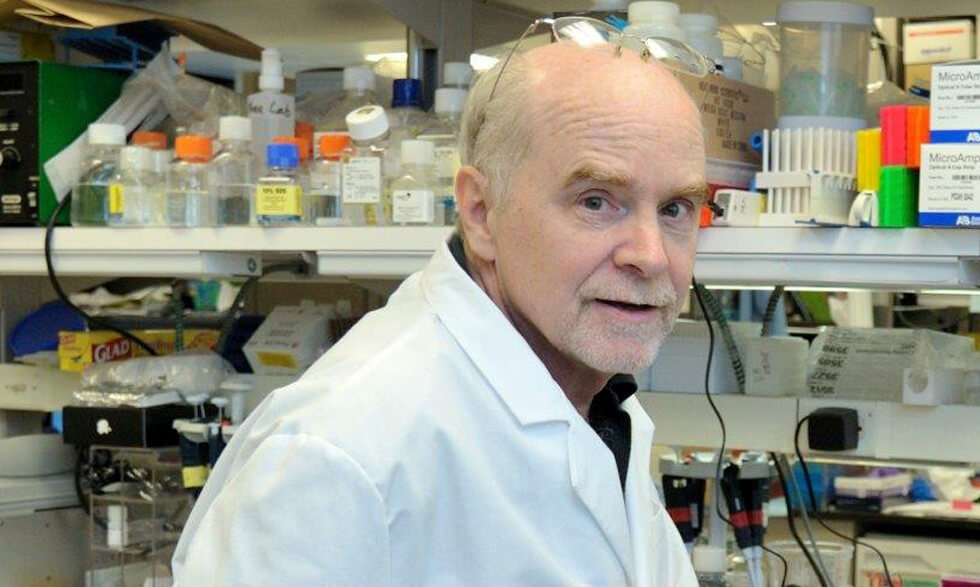
- John O'Shea, M.D.
These can help slow or stop joint damage, minimize disability, and reduce inflammation, pain and swelling. Lowering, stress, eating a healthy diet, quitting smoking, and getting enough rest are all suggested lifestyle changes.
Some medicines are taken by mouth, while others require regular injections; these drugs are highly effective, but do have side effects. Thus, it's essential to get a proper diagnosis from a doctor who specializes in rheumatic diseases, understands all the different causes of arthritis—in adults and children—and has experience with the new drugs, advises John O'Shea, M.D., scientific director at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS).
"RA and other autoimmune diseases don't just affect the joints, they cause inflammation throughout your body," Dr. O'Shea says.
The main goal in treating RA is to reduce inflammation and pain, stop more joint damage, and to be able to function normally.
"We now have better treatment therapies to keep you safe, as well as clinical studies that specifically look at inflammation," Dr. O'Shea adds. The RA drug tofacitinib, approved for the treatment of RA in 2012, targets a protein that was discovered in the early 1990s by O'Shea and his colleagues.
Dr. O'Shea and his team at NIAMS are studying the molecular and genetic basis of rheumatoid arthritis and other inflammatory diseases in an effort to identify potential strategies for future therapies.
Researchers are also studying the natural history of the disease in children and adults to understand more fully how RA progresses and impacts people's lives.
In addition, NIAMS researchers are collaborating with investigators outside of NIH to explore whether people with RA who are in remission (no symptoms of the disease) while taking TNF inhibitors are at risk of having symptoms come back if they stop taking the medicine.
Another study funded by NIAMS focuses on RA patients with inflammation in the blood vessels and heart tissue, which can eventually lead to heart disease.
"People who have rheumatoid arthritis have a 50 percent increase in chance of experiencing a stroke or heart failure," says Joan Bathon, M.D., chief of the division of rheumatology at Columbia University Medical Center in New York.
Known as the TARGET study, the clinical trial aims to see if treatment of arthritis in individuals with RA will also reduce inflammation in blood vessels. Inflammation in blood vessels is believed to be an early predictor of atherosclerosis (hardening of the arteries) which leads to heart attacks and strokes. If RA medications reduce inflammation in blood vessels, this may reduce future chances of heart attacks and strokes. "We want to aggressively treat rheumatoid arthritis, to see if it will help the heart," Dr. Bathon says.
Joining a clinical study such as the TARGET study will help researchers find a cure more quickly. There are 30 sites in the U.S. focusing on the TARGET study, with more to come soon.
"We have a lot of treatments, but none of our treatments cure the disease," Dr. Bathon says. "In lieu of a cure is prevention of related complications from the disease. RA is treatable. We're focusing on outcomes right now and getting people with RA back on track."
The bottom line: If you have symptoms of rheumatoid arthritis, early diagnosis is essential. It is critical to get aggressive treatment as early as possible to help slow RA and help prevent permanent joint damage.