Colorectal cancer is the third leading cause of cancer-related deaths among men and women in the United States, with 151,030 new cases estimated to occur this year. "Colorectal cancer" can refer to any cancer that forms in the tissue that lines the inside of the colon or rectum. While some people are at higher risk than others, anyone can get colorectal cancer. Screening is important to detect the disease and remove precancerous polyps before they become cancerous.
What are the symptoms of colorectal cancer?
The following symptoms can be caused by other conditions, but people experiencing them should consult their doctor:
- Diarrhea or constipation
- A feeling that your bowel does not empty completely
- Blood in your stool
- Stools that are narrower than usual
- Frequent gas pains or cramps
- Frequently feeling full or bloated
- Weight loss with no known reason
- Fatigue
- Nausea or vomiting
Who is at risk for colorectal cancer?
While anyone can get colorectal cancer, the National Cancer Institute (NCI) reports that slightly more than 1 in 25 men and women will develop colorectal cancer in their lifetime.
People who have had colorectal cancer in the past or who have had certain kinds of colorectal polyps removed are at greater risk for developing colorectal cancer, as are those with a family history of the disease. People with Lynch syndrome or familial adenomatous polyposis, both of which are inherited conditions, or who have a history of inflammatory bowel disease such as ulcerative colitis or Crohn’s disease are also at higher risk.
Some lifestyle factors associated with increased risk include excessive alcohol consumption, obesity, smoking, and possibly diet.
Rates of colorectal cancer are also higher for Black people and non-Hispanic American Indians/Alaska Natives than any other racial or ethnic groups.
As you get older, your risk increases. The U.S. Preventive Services Task Force recommends colorectal cancer screening for adults ages 45 to 75 of average risk. Screening for patients ages 76 to 85 is recommended for select individuals. Colorectal cancer is still rare among adults younger than 50, but these rates are increasing. You should consult your doctor about screening methods and frequency.
How is colorectal cancer screened?
Colorectal cancer is detected using a range of procedures, some invasive and some not. These include colonoscopies, stool tests, and sigmoidoscopies. Abnormalities, including lesions or polyps found during a screening, will be tested for cancer. A new approach is to check blood samples for genetic material that polyps or tumors may release into the bloodstream.
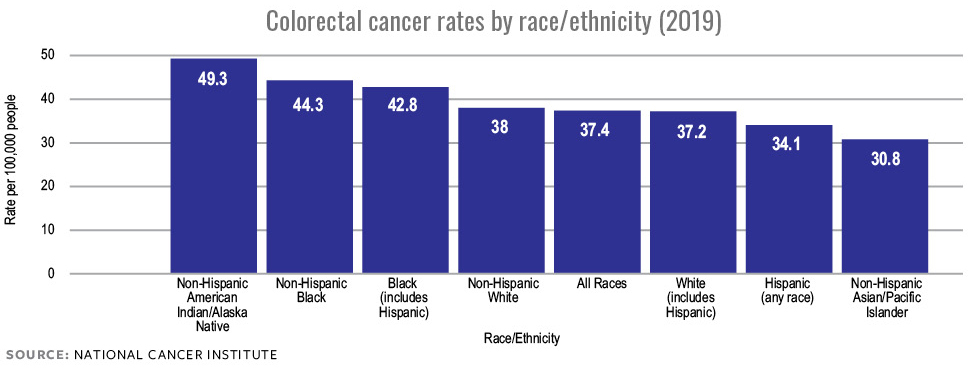
Colorectal cancer rates by race/ethnicity.
How is colorectal cancer treated?
Treatment for colorectal cancer depends on the type and stage of a person’s disease and may be combined. Standard treatments include:
- Surgery. This can be to remove polyps, cancer, or part or all of the colon or rectum depending on the cancer’s spread and stage.
- Chemotherapy. Powerful chemicals administered intravenously (with an IV) or orally (swallowing capsules or pills) kill fast-growing cancer cells in the body.
- Targeted therapy. A drug delivered intravenously or orally targets the proteins that control how cancer cells grow, divide, and spread.
- Radiofrequency ablation. A probe inserted into the body emits radiofrequency waves to the tissue around a growth. The cells in that tissue die and the immune system removes them, which causes the growth to shrink.
- Cryosurgery. Liquid nitrogen applied to the growth freezes its cells, causing them to die and to be absorbed into the body.
- Radiation therapy. High doses of radiation damage cancer cells’ DNA, causing them to die over time.
- Immunotherapy. This treatment harnesses the body’s immune system to control and eliminate cancer. Drugs are usually administered intravenously.
If your doctor finds colorectal cancer, they may recommend more tests to see whether the disease has spread to other parts of the body. Colorectal cancer can spread through tissue, the lymph system (organs that help fight infections and move fluid through the body), or the blood. This development is called metastatic cancer and is the most advanced stage.
NCI has several resources available, including a list of questions you may want to ask your doctor if they recommend treatment for colorectal cancer. It’s important to talk to your doctor about not only what will happen during the treatment itself but possible side effects and how any other medications, dietary supplements, or drugs you may be taking could affect the treatment.
Remember that colorectal cancer can come back even after being treated. It’s important to continue the screenings your doctor recommends so they can restart treatment if the disease returns.
Coping with colorectal cancer
If you or a loved one are diagnosed with colorectal cancer, you are not alone! NCI has information for both patients and caregivers about managing and recovering from colorectal cancer, including questions to ask your doctor and how to connect with support groups.
Current NCI research on colorectal cancer
Several projects are underway with support from the National Cancer Institute, including:
The ACCSIS program
As part of the Cancer MoonshotSM, the ACCSIS (Accelerating Colorectal Cancer Screening and follow-up through Implementation Science) program comprises eight research projects to increase the rates of colorectal cancer screenings, follow-ups, and referrals to care. ACCSIS has a special focus on racial and ethnic minority populations, rural communities and difficult-to-reach areas, and other underserved groups. Read more about the ACCSIS project.
FORTE Colorectal Cancer Prevention Trial
People ages 50 to 69 who have had one or two small, noncancerous polyps completely removed during a colonoscopy within the past four years may qualify to participate in the FORTE (Five- or Ten-Year Colonoscopy for 1-2 Non-Advanced Adenomatous Polyps) study. This research aims to help determine how long such people can wait for a follow-up screening after a routine colonoscopy. Read more about this study.
COMMIT study for colorectal cancer treatment
COMMIT (Combination Chemotherapy, Bevacizumab, and/or Atezolizumab in Treating Patients with Deficient DNA Mismatch Repair Metastatic Colorectal Cancer) is a nationwide study that looks at a combination of treatments for people with metastatic colorectal cancers whose tumors are deficient in DNA mismatch repair. Read more about this study, including eligibility requirements for participating.