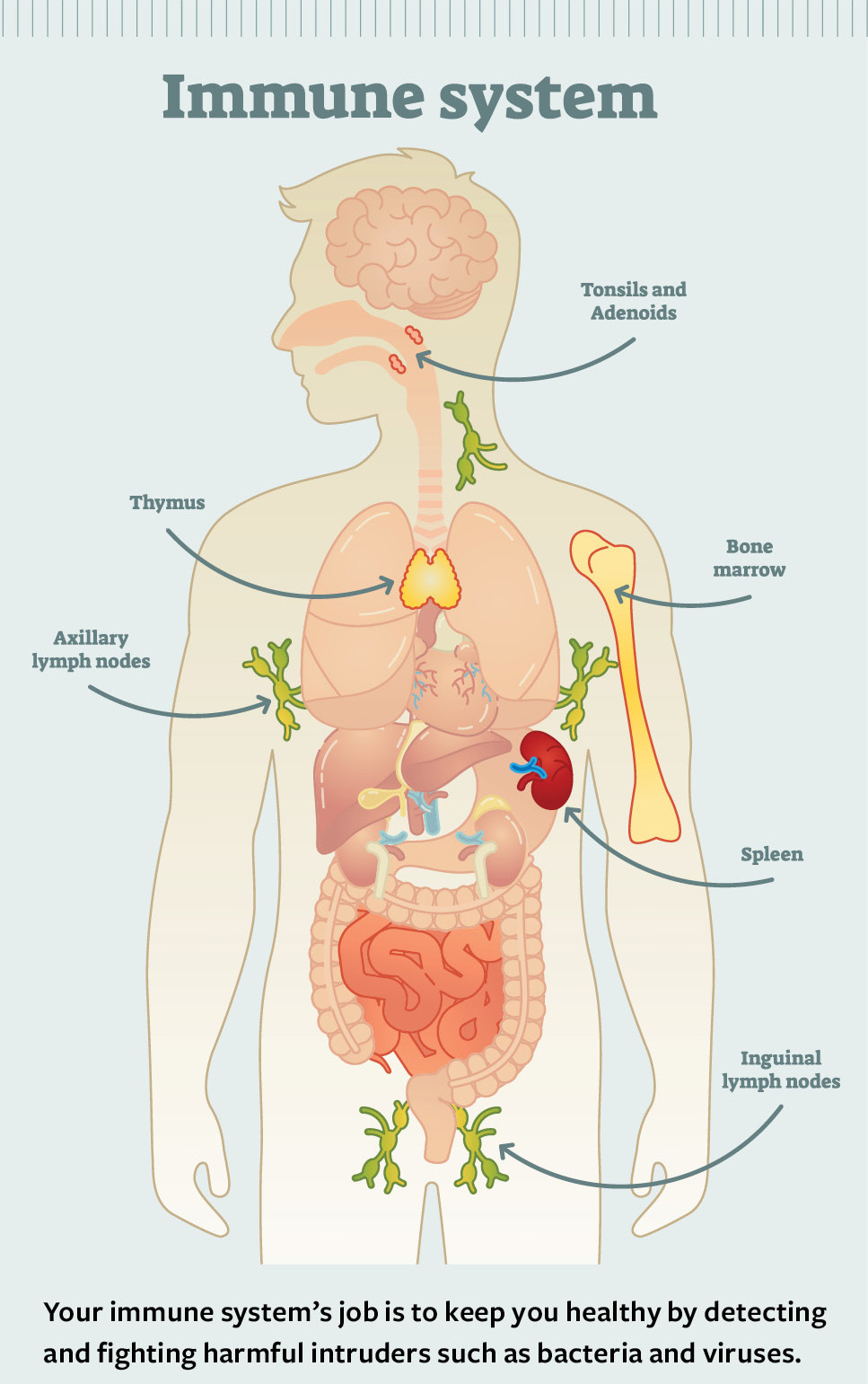
Your immune system’s job is to keep you healthy by detecting and fighting harmful intruders such as bacteria and viruses. If you have an autoimmune disease, your immune system mistakenly attacks your body’s healthy cells, tissues, and organs.
There’s no cure for autoimmune diseases—at least not yet—but there are treatments to help manage their symptoms. Getting diagnosed and starting treatment as soon as possible can help prevent more severe damage further down the road.
How do autoimmune diseases work?
The immune system is a network of cells and organs that work together to fight infections and protect the body against diseases. For example, the skin and mucus membranes help prevent harmful germs from entering the body, and the organs and tissues of the lymphatic system (including the spleen, tonsils, thymus gland, bone marrow, and lymph nodes) create and store the white blood cells that fight infection.
In a healthy immune response, the immune system creates lymphocytes (a type of white blood cell) and antibodies (protective proteins) that identify unfamiliar substances called antigens and attack them to protect the body.
Typically, the immune system can tell the difference between the body’s own cells and tissues and potentially harmful intruders such as viral and bacterial antigens. In people with autoimmune conditions, the immune system gets confused and produces autoantibodies, a type of antibody that attacks healthy cells and tissues. This can lead to inflammation in different parts of the body, harm the body’s organs and systems, and contribute to a wide range of symptoms.
What are the different types of autoimmune diseases?
There are more than 80 known autoimmune conditions, which together affect more than 23.5 million Americans. Each disease is different, but what they all have in common is a haywire immune response that turns the immune system against the body it is supposed to protect.
Some conditions target specific organs or tissues, such as the skin, heart, or blood vessels. Others are more general, targeting multiple tissue or organ systems throughout the body.
Examples of common organ-specific conditions include type 1 diabetes (pancreas), inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis (digestive tract), and multiple sclerosis (brain and spinal cord). Systemic conditions—those that attack multiple systems—include systemic lupus erythematosus, also known as lupus or SLE, Sjögren’s syndrome, and scleroderma, which all affect tissues and organs throughout the body.
What causes them?
While scientists and doctors aren’t exactly sure what causes autoimmune disease, they are likely triggered by interactions between genes, the immune system, and the environment.
There’s still a lot to learn about these relationships, but experts think that even if a person with certain genes or certain combinations of genes is at risk of an autoimmune disease, they probably won’t develop the condition without something in their environment triggering it or turning it on. Environmental triggers may include:
- Infection (from a virus or bacteria)
- Stress
- Dietary components (such as gluten or dairy)
- Contaminants in food (such as mercury in fish)
- Environmental pollutants (such as certain pesticides)
Who is at risk?
Autoimmune diseases tend to run in families. You’re more likely to develop one if you:
- Have a family member with an autoimmune disease
- Are already diagnosed with one or more autoimmune diseases
Also, your racial and ethnic background, assigned sex, and age may make you more or less likely to develop certain autoimmune diseases. For example, many kinds of autoimmune diseases such as lupus, scleroderma, and Sjögren’s syndrome are far more common among women than among men.
Because specific viruses or environmental conditions may trigger autoimmune diseases, the risk of certain autoimmune diseases may be higher in people who are more likely to be exposed to those triggers.
What are the symptoms?
Autoimmune diseases can affect different parts of the body. Their symptoms can be similar and even vague, and specific symptoms may not even look the same for every condition. Many of the most common ones―such as fatigue, joint pain, and muscle pain―could also be symptoms of other conditions.
Most autoimmune diseases cause inflammation, so people with autoimmune diseases often experience heat, pain, or swelling (which are all signs of inflammation) in the part of the body that’s affected. Other common symptoms include:
- Fatigue
- Low-grade fever
- Losing or gaining weight
- Dizziness
- Swelling or pain in muscles or joints
- Difficulty thinking clearly or paying attention
- Rashes
- Digestive problems (such as bloating, cramping, diarrhea, or constipation)
People with autoimmune conditions often experience symptoms in cycles, and symptoms can change over time. Even with treatment, there may be periods of time where symptoms worsen or new symptoms appear (flares), followed by periods of remission where they disappear or become less intense.
How are autoimmune diseases diagnosed?
For many people with autoimmune symptoms, getting an accurate diagnosis can be difficult, time-consuming, and stressful.
To diagnose an autoimmune disease, a health care provider will do a physical exam and ask you about your symptoms, your medical history, and your family’s health history, including if others in your family have been diagnosed with one or more autoimmune diseases. Depending on your symptoms and background, they may recommend blood tests, imaging, or other diagnostic tests.
How are they treated?
There’s no cure for most autoimmune diseases, but there are treatments to help people who have them address and manage their symptoms. Treatments vary depending on the disease and how the individual is affected.
In addition to your primary care provider, you may work with one or more specialists, including:
- Immunologists (for immune system disorders)
- Rheumatologists (for rheumatic diseases such as arthritis and other inflammatory disorders)
- Endocrinologists (for glands and hormones)
- Hematologists (for blood disorders)
- Neurologists (for nervous system disorders)
- Cardiologists (for diseases of the heart and blood vessels)
- Gastroenterologists (for the gastrointestinal tract)
- Dermatologists (for skin diseases)
You and your health care team can work together to create a treatment plan that works best for you, your lifestyle, and your symptoms with the fewest possible side effects. This could include pharmacological (drug-based) medicines that:
- Reduce pain (such as nonsteroidal anti-inflammatory drugs)
- Control inflammation (such as corticosteroids)
- Inhibit the immune response (such as immunosuppressants)
In addition to these treatments, there may be certain activities, diets, and long-term lifestyle changes that can help you manage your symptoms and feel better.